Sterilization is the silent backbone of molecular biology and biotechnology research. While often taken for granted, the processes and mechanisms that underpin effective sterilization remain an area of active scientific investigation. Understanding what steam sterilization truly achieves—and where its limits lie—is essential for labs seeking rigor, reproducibility, and safety in high-stakes research environments.
How Sterilization Works: From Vegetative Cells to Spores
Steam sterilization inactivates microorganisms primarily through protein denaturation and nucleic acid damage caused by high temperature and saturated steam under pressure. While vegetative bacteria, fungi, and viruses are generally inactivated rapidly at 121 °C for 15–20 minutes, spores of thermophilic bacteria—such as Geobacillus stearothermophilus—are far more resistant.
Recent studies have examined the molecular basis of spore resistance. Proteins within the spore core, high levels of calcium dipicolinate, and specialized DNA-binding proteins protect spores against heat and desiccation. Research published in Frontiers in Microbiology (2022) shows that even small reductions in steam saturation or trapped air pockets can allow spores to survive, underscoring the importance of precise temperature, pressure, and steam penetration for complete sterilization.
“Spores are not simply dormant—they have evolved multi-layered defenses against extreme heat, making sterilization validation a non-negotiable step in high-reliability labs.”
— Dr. Maria Chen, Microbial Resistance Researcher, University of California
Beyond Bacteria: Prions, Biofilms, and Emerging Challenges
Sterilization research is increasingly focused on biologically challenging targets:
- Prions: Highly resistant misfolded proteins require more aggressive sterilization conditions, often exceeding 134 °C with prolonged exposure or chemical pre-treatment. Standard 121 °C cycles are insufficient, which has implications for tissue handling in clinical and research settings.
- Biofilms: Microbial communities embedded in extracellular matrices exhibit increased thermal resistance. Recent work in Applied and Environmental Microbiology (2021) shows that spores embedded in biofilms can survive standard autoclave cycles if steam penetration is incomplete.
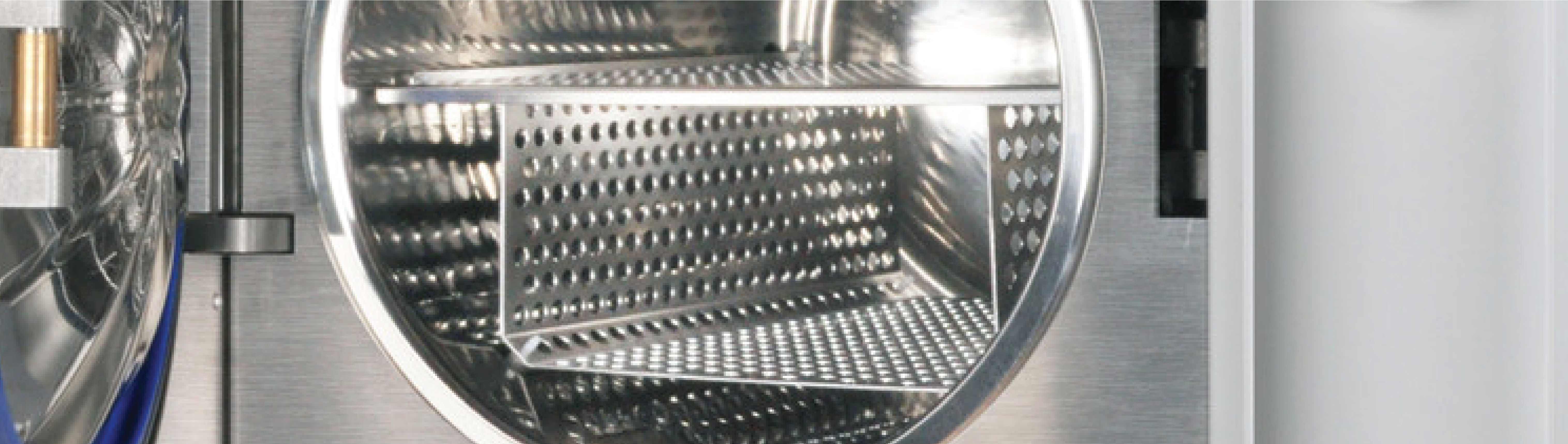
These findings highlight that even well-designed sterilization cycles can fail under non-ideal conditions, emphasizing the need for empirical validation in research-grade autoclaves.
Validation Science: Measuring What Sterilization Achieves
Modern studies explore not just whether sterilization occurs, but how efficiently and uniformly it occurs. Key areas of research include:
- Biological indicators (BIs): The use of G. stearothermophilus spores to test lethality remains standard. Quantitative studies demonstrate that BI placement at cold spots in flasks or wrapped instruments reveals vulnerabilities in steam distribution.
- Cold-point and thermal mapping: Data loggers and thermocouples are now used to model heat penetration inside complex loads. Research in Journal of Applied Microbiology (2020) shows that load geometry can create temperature differences of several degrees, potentially compromising spore inactivation.
- Predictive modeling: Computational models simulate steam flow and heat transfer in chamber designs. These models allow researchers to optimize cycle times and predict lethality without relying solely on trial-and-error, improving both reproducibility and safety.
Sterilization and Material Integrity
Another frontier of sterilization research addresses the impact on lab materials and reagents. While autoclaving ensures sterility, repeated cycles can affect polymers, media containers, and even some biomolecules.
Studies in MDPI Polymers (2021) indicate that repeated steam exposure may alter mechanical properties of polycarbonate and polypropylene labware, including:
- Slight reductions in tensile strength and impact resistance
- Clouding or loss of transparency
- Minor warping after multiple cycles
These insights are particularly relevant for labs striving to balance reusability, sustainability, and experimental consistency.
Emerging Questions in Sterilization Science
The field continues to evolve. Current research questions include:
- Can ultrafast or pulsed sterilization cycles achieve comparable lethality with lower energy consumption?
- How does steam sterilization affect molecular reagents or nucleic acids in contact with sterilized glassware or instruments?
- What are the best strategies to verify sterility in biofilm-rich or high-biomass environments without overloading the autoclave?
These studies not only push forward sterilization science but also inform how labs design protocols, validate equipment, and minimize contamination risk.
Conclusion
Steam sterilization remains a cornerstone of molecular biology, biotechnology, and clinical research. Yet, as studies continue to reveal, the process is far from trivial. Spores, prions, biofilms, and material sensitivities all present challenges that demand rigorous validation, monitoring, and understanding of underlying mechanisms. For labs seeking to combine safety, reliability, and operational efficiency, reviewing advanced autoclaves—such as the Benchmark Scientific B4000-28 Research Autoclave—can provide the precise control and proven performance necessary to meet these challenges.
Sources
- CDC (2023). Guidelines for Disinfection and Sterilization in Healthcare Facilities.
- Frontiers in Microbiology (2022). Mechanisms of Bacterial Spore Resistance to Heat.
- Applied and Environmental Microbiology (2021). Thermal Resistance of Biofilm-Embedded Spores.
- MDPI Polymers (2021). Effects of Repeated Autoclave Cycles on Polymeric Labware.
- Certoclav. Steam Sterilization Temperature and Pressure Parameters.